In the realm of insurance, navigating the claims process can be akin to traversing a labyrinth. As a policyholder, you entrust your hopes and expectations to the hands of insurers, eagerly anticipating a seamless and efficient resolution. However, keeping track of your submitted claims can often feel like chasing shadows in the dark.
Fear not, for we have assembled a comprehensive guide to illuminate your path through the intricacies of claim tracking. With these invaluable tips, you’ll transform from a bewildered wanderer into a confident navigator, ensuring your claims receive the attention and progress they deserve.
Claim Tracking Methods
Insurance claim tracking is crucial to ensure timely processing and reimbursement. Various methods are available, each with unique advantages and disadvantages. This section provides an overview of popular claim tracking methods, including online portals, mobile apps, and third-party software.
Online Portals
Insurance companies often offer online portals for policyholders to track their claims. These portals allow users to view the status of their claim, submit supporting documents, and communicate with the insurance company.
Pros:
- Convenience: Accessible from anywhere with an internet connection.
- Security: Secure login and encryption ensure data privacy.
- Transparency: Real-time updates and detailed claim information.
Cons:
- Limited functionality: Some portals may not offer all necessary features.
- Technical issues: Occasional glitches or outages may affect accessibility.
Mobile Apps
Insurance companies are increasingly developing mobile apps that provide claim tracking capabilities. These apps offer similar functionality to online portals but with the added convenience of being accessible on smartphones.
Pros:
- Convenience: Easy access anytime, anywhere, using a smartphone.
- Push notifications: Real-time updates and reminders on claim status.
- Photo submission: Easily upload photos of supporting documents.
Cons:
- Limited functionality: Some apps may have fewer features than online portals.
- Data usage: Using the app may consume cellular data, leading to additional charges.
Third-Party Software
Third-party software solutions are available for claim tracking. These tools offer advanced features and integrations with various insurance companies.
Pros:
- Comprehensive features: Robust functionality, including claim submission, tracking, and reporting.
- Integration: Connects with multiple insurance companies for centralized tracking.
- Customization: Tailored to specific business needs and workflows.
Cons:
- Cost: Third-party software may come with subscription fees.
- Implementation: Requires setup and training, which can be time-consuming.
The choice of claim tracking method depends on individual preferences, the features required, and the level of convenience desired. It’s essential to evaluate the pros and cons of each method to select the one that best suits the specific needs and requirements.
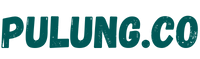
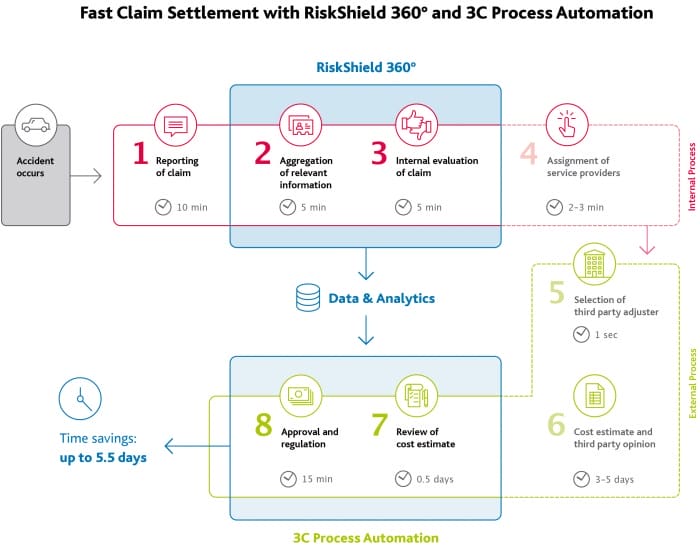
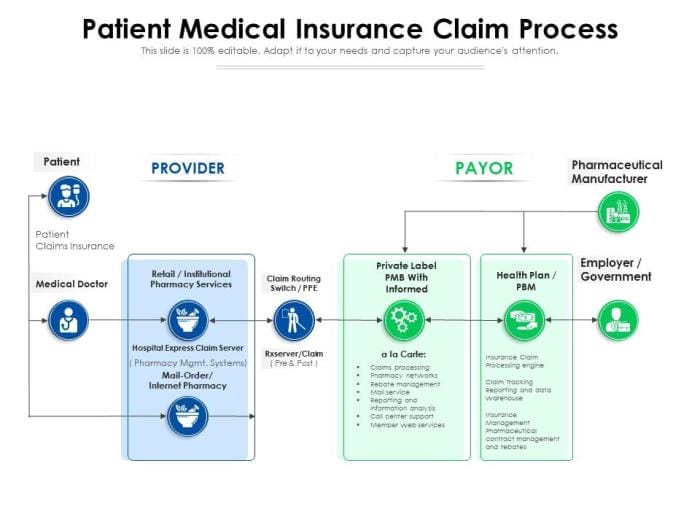
Claim Submission Process
The claim submission process is a series of steps taken by an insured individual or organization to notify the insurance company about a covered loss and seek reimbursement for the damages incurred. Understanding the process and following the necessary steps can expedite the claim settlement and ensure a smooth resolution.
The claim submission process typically involves the following stages:
Initial Notification
The first step in the claim submission process is to notify the insurance company about the covered loss. This can be done through various channels, such as:
- Calling the insurance company’s customer service number.
- Submitting a claim online through the insurance company’s website.
- Visiting the insurance company’s local office.
- Sending a written notice to the insurance company’s mailing address.
When making the initial notification, be prepared to provide the following information:
- Your name, policy number, and contact information.
- The date, time, and location of the covered loss.
- A brief description of the covered loss.
- Any relevant documentation or evidence supporting the claim.
Claim Form Submission
Once the insurance company has received the initial notification, they will typically send you a claim form. This form will require you to provide more detailed information about the covered loss, including:
- The cause of the covered loss.
- The extent of the damages incurred.
- An estimate of the repair or replacement costs.
- Any additional documentation or evidence supporting the claim.
It is important to complete the claim form accurately and thoroughly. Providing incomplete or inaccurate information can delay the claim settlement process.
Investigation and Assessment
Once the insurance company receives the completed claim form, they will typically assign an adjuster to investigate the claim. The adjuster will contact you to gather additional information and inspect the damaged property.
The adjuster will also work with you to determine the cause of the covered loss and the extent of the damages incurred. They will use this information to assess the value of the claim and determine the amount of reimbursement that you are entitled to.
Settlement and Payment
Once the insurance company has completed its investigation and assessment, they will issue a settlement offer. This offer will typically include a check for the amount of reimbursement that you are entitled to.
If you accept the settlement offer, you will need to sign a release form. This form will release the insurance company from any further liability for the covered loss.
If you disagree with the settlement offer, you can appeal the decision. The appeals process will vary depending on the insurance company.
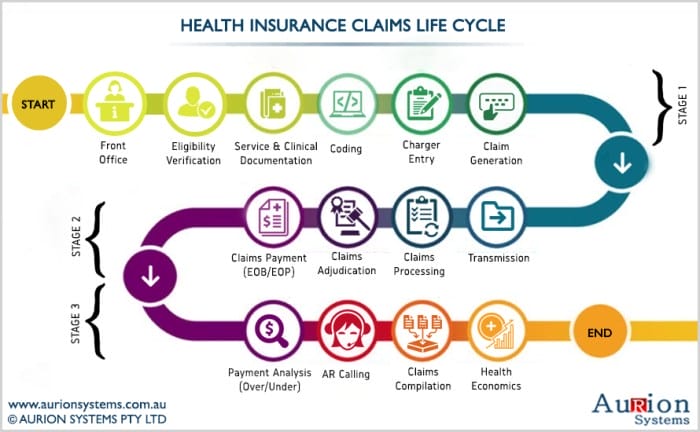
Claim Status Updates
Establishing a robust system for tracking claim status is essential for efficient claims processing and policyholder satisfaction. This system should provide real-time updates and notifications to ensure transparency and prompt communication throughout the claim journey.
Proactive communication with policyholders is paramount in managing their expectations and fostering trust. Regular updates on claim progress, potential delays, and necessary documentation help policyholders stay informed and engaged in the process.
Real-Time Updates and Notifications
- Implement an online portal or mobile app that allows policyholders to access their claim status 24/7.
- Enable automated notifications via email, SMS, or push notifications to keep policyholders informed of any updates or changes in claim status.
- Provide a dedicated customer service hotline or live chat option for policyholders to directly inquire about their claim status.
Proactive Communication
- Assign a dedicated claims representative to each policyholder to serve as a single point of contact throughout the claim process.
- Regularly communicate with policyholders, providing updates on the status of their claim, any required documentation, and potential delays.
- Be transparent and honest in communication, addressing any concerns or questions policyholders may have promptly and professionally.
Claim Documentation
Proper documentation is crucial for a successful insurance claim. Providing comprehensive and organized records enhances the claim review process, ensuring a prompt and accurate settlement.
To facilitate a seamless claim submission, ensure you have the following essential documents:
Personal Information
- Policyholder’s Name: Full legal name as stated in the insurance policy.
- Contact Information: Current address, phone numbers, and email address.
- Social Security Number or Taxpayer Identification Number: For identification purposes.
Policy Details
- Policy Number: Unique identifier assigned to the insurance policy.
- Policy Type: Whether it’s auto, home, health, or any other type of insurance.
- Coverage Details: Explanation of the specific coverage limits and exclusions.
- Premium Payment Records: Proof of premium payments, including receipts or bank statements.
Supporting Evidence
- Proof of Loss: Detailed description of the incident or event leading to the claim, including date, time, and location.
- Police Report: In case of accidents or theft, a copy of the official police report is necessary.
- Medical Records: For health insurance claims, provide medical records, prescriptions, and bills related to the treatment.
- Property Damage Estimates: For property damage claims, obtain estimates from qualified professionals.
- Photographs: Visual documentation of the damage or loss, including close-ups and wide shots.
- Receipts and Invoices: For reimbursement claims, attach receipts and invoices related to the expenses incurred.
Organizing these documents systematically in a designated folder or digital file makes the claim submission process more efficient and streamlines the review by the insurance company.
Claim Timeline Management
![]()
Efficient claim timeline management ensures prompt claim processing and timely resolution. It involves setting realistic expectations, tracking milestones, and communicating timeline updates effectively to policyholders and stakeholders.
Establishing Realistic Timelines
Setting realistic claim timelines is crucial to managing expectations and avoiding delays. Factors to consider include the complexity of the claim, the availability of necessary documentation, and the involvement of multiple parties. Setting achievable timelines fosters trust and credibility with policyholders.
Tracking Milestones
Regularly tracking claim milestones helps identify potential bottlenecks and ensures timely progress. This can be done through claim tracking software, spreadsheets, or manual methods. Monitoring milestones enables proactive intervention to address any issues or delays promptly.
Communicating Timeline Updates
Proactively communicating timeline updates to policyholders and stakeholders is essential to maintain transparency and manage expectations. This can be done through regular emails, phone calls, or online portals. Clear and timely communication builds trust and reduces anxiety among policyholders.
6. Communication Channels
![]()
The success of your insurance claim submission process heavily depends on your communication with the insurance company. It’s essential to use the right communication channels to ensure that your claim is processed quickly and efficiently. In this section, we’ll discuss the advantages and disadvantages of different communication channels that policyholders can use to submit and track claims.
Phone Calls
Phone calls are a direct way to reach a customer service representative who can assist you with your claim. This channel offers the advantage of real-time interaction, allowing you to ask questions, clarify doubts, and receive immediate feedback. However, phone calls might face long wait times, especially during peak hours.
Additionally, if you have language barriers or prefer written communication, phone calls might not be the best option.
Emails
Emails provide a written record of your communication with the insurance company. They offer convenience, allowing you to send your claim submission or inquiry outside of business hours. Emails are also helpful for attachments like supporting documents or images. However, email communication can be slower than phone calls, and it might take several days for a response.
Moreover, if you have urgent needs, relying solely on email communication might lead to delays.
Online Forms
Many insurance companies have dedicated online forms for submitting claims. These forms are usually easy to use and allow you to input all the necessary information at once. Online forms are convenient, allowing you to submit a claim from the comfort of your home or office.
However, the disadvantage is that you might miss out on the personalized attention that you might get with phone calls.
Social Media
Social media platforms can be used to communicate with insurance companies, especially for inquiries or general feedback. The advantage of social media is that it allows for quick and public communication. However, it’s not the most suitable channel for in-depth claim submissions or tracking.
Social media might be best used as a supplementary channel for general inquiries or feedback.
Claim Resolution Process

The claim resolution process encompasses a series of steps undertaken by insurance companies to assess, evaluate, and settle insurance claims filed by policyholders. The process begins with the initial assessment of the claim and culminates in the final settlement or denial of the claim.
The efficiency and effectiveness of the claim resolution process play a crucial role in ensuring policyholder satisfaction and maintaining trust in the insurance industry. Various factors influence the claim resolution timeline, including the complexity of the claim, the availability of necessary documentation, and the insurer’s internal processes and resources.
Factors Influencing Claim Resolution Timelines
- Claim Complexity: Complex claims involving multiple parties, extensive damages, or specialized expertise may require additional time for investigation and assessment.
- Documentation Availability: The timely submission of complete and accurate documentation, such as claim forms, medical records, and police reports, can expedite the claim resolution process.
- Insurer’s Internal Processes: The efficiency of the insurer’s claim handling procedures, including the availability of resources and the expertise of claim adjusters, can impact the resolution timeline.
- Communication and Cooperation: Effective communication between the policyholder, insurer, and any third parties involved in the claim can facilitate a smoother and more efficient resolution process.
Claim Reporting Requirements
Insurance claims reporting is a crucial aspect of claim management. It involves meeting regulatory compliance standards and maintaining internal documentation to ensure accurate and timely reporting.
Effective claim reporting ensures that all necessary information is captured, reviewed, and communicated to the appropriate parties. It also helps in identifying trends, improving claim handling processes, and ensuring that claims are resolved efficiently.
Regulatory Compliance
Insurance companies are required to comply with various regulations and guidelines set by government agencies and industry associations. These regulations Artikel the specific requirements for reporting insurance claims, including the format, content, and timeframe for submission.
- Failure to comply with these regulations can result in penalties, fines, and reputational damage.
- Insurance companies must have a clear understanding of the reporting requirements and establish processes to ensure compliance.
Internal Documentation
In addition to regulatory compliance, insurance companies also need to maintain internal documentation of insurance claims. This documentation serves as a record of the claim, including the details of the incident, the investigation process, and the resolution.
- Internal documentation is essential for claims auditing, risk management, and improving claim handling processes.
- Insurance companies should have a standardized approach to internal claim documentation, ensuring consistency and accuracy.
Checklist for Claim Reports
To ensure that claim reports are complete and accurate, insurance companies should use a checklist that includes the following essential information:
- Policyholder information (name, address, policy number)
- Details of the incident (date, time, location)
- Description of the loss or damage
- Estimated cost of the loss or damage
- Contact information for witnesses and other relevant parties
- Supporting documentation (photos, receipts, police reports)
Claim Fraud Detection
Insurance claim fraud is a growing problem that costs insurance companies billions of dollars each year. It can also lead to higher premiums for policyholders. There are many different types of insurance claim fraud, but some of the most common include:
- Staged accidents: This is when two or more people work together to cause an accident, usually a car accident, in order to collect insurance money.
- Exaggerated claims: This is when a policyholder intentionally inflates the value of their claim in order to get a larger payout from their insurance company.
- False claims: This is when a policyholder files a claim for damages or losses that never actually happened.
- Identity theft: This is when someone uses another person’s name and personal information to file a fraudulent insurance claim.
Insurance companies use a variety of methods to detect fraudulent claims. These methods include:
- Investigating claims: Insurance companies will often investigate claims that seem suspicious. This may involve talking to witnesses, reviewing police reports, and inspecting the damaged property.
- Using data analytics: Insurance companies use data analytics to identify patterns of fraud. For example, they may look for claims that are filed from the same address or phone number multiple times.
- Working with law enforcement: Insurance companies often work with law enforcement to investigate and prosecute insurance fraud. This can lead to criminal charges for the people involved in the fraud.
Policyholders can protect themselves from fraudulent claims by:
- Being aware of the different types of insurance fraud.
- Being careful about who they give their personal information to.
- Reporting any suspicious activity to their insurance company.
Claim Analytics and Reporting
Understanding claim data is essential for identifying patterns, trends, and insights that can help improve claim handling processes, reduce costs, and enhance customer satisfaction. A robust claim analytics and reporting system provides valuable information to stakeholders, including claims managers, underwriters, and executives.
Data Collection and Analysis
The foundation of claim analytics is the collection and analysis of claim-related data. This data includes information such as claim type, date of loss, cause of loss, amount paid, and claim status. By analyzing this data, insurers can identify common claim patterns, high-risk areas, and potential fraud.
Dashboard and Reporting System
A well-designed dashboard or reporting system is crucial for visualizing and analyzing claim-related information. This system should provide interactive features that allow users to drill down into the data, filter results, and generate custom reports. The dashboard should also include key performance indicators (KPIs) that measure the effectiveness of the claim handling process.
Claims Analytics Applications
Claim analytics can be used in various ways to improve claim handling processes. Some common applications include:
- Identifying Fraud: Claim analytics can help identify suspicious claim patterns that may indicate fraud. For example, a high number of claims from the same policyholder or claims with similar characteristics may warrant further investigation.
- Managing Catastrophic Losses: Claim analytics can assist insurers in managing catastrophic losses by identifying areas at high risk of natural disasters or other catastrophic events. This information can be used to develop mitigation strategies and allocate resources accordingly.
- Improving Customer Service: Claim analytics can help insurers improve customer service by identifying areas where the claim handling process can be streamlined or improved. For example, analytics can identify delays in claim processing or areas where communication with policyholders can be enhanced.
Conclusion
Claim analytics and reporting are powerful tools that can help insurers improve claim handling processes, reduce costs, and enhance customer satisfaction. By leveraging data and technology, insurers can gain valuable insights into their claim portfolio and make informed decisions to improve their operations.
Last Word
As you embark on this journey, remember that knowledge is your most potent weapon. Equip yourself with the insights provided in this guide, and you’ll emerge as a master of claim tracking, leaving the uncertainties behind. Embrace proactive communication, leverage technology, and maintain meticulous records.
By doing so, you’ll transform the claims process from a daunting maze into a clear and manageable path, leading to a swift and satisfactory resolution.
FAQ Section
Q: What is the most efficient method for tracking insurance claims?
A: While personal preferences may vary, online portals often provide a user-friendly interface, real-time updates, and secure access to claim information. They eliminate the need for phone calls or visits to insurance offices, offering convenience and efficiency.
Q: How can I ensure my claim is processed promptly?
A: Submitting complete and accurate documentation from the outset is crucial. Meticulously review the list of required documents and ensure you provide everything necessary. This proactive approach minimizes the need for additional requests and expedites the claim processing timeline.
Q: How can I stay updated on the status of my claim?
A: Many insurance companies offer online claim tracking systems that allow you to check the status of your claim in real-time. These systems typically provide detailed information about the claim’s progress, including any outstanding requirements or approvals needed.
Q: What should I do if I have questions or concerns about my claim?
A: Do not hesitate to contact your insurance company directly. They have dedicated customer service representatives who are knowledgeable about the claims process and can provide assistance. Clearly articulate your questions or concerns, and be prepared to provide relevant information about your claim.