When faced with the necessity of root tip removal, understanding the intricacies of dental insurance coverage can be a daunting task. This procedure, often performed to address infection, decay, or trauma, involves the surgical extraction of a tooth’s remaining root tip.
In this comprehensive guide, we delve into the nuances of dental insurance coverage for root tip removal, exploring factors that influence coverage, pre-approval processes, and strategies for handling denied claims.
Delving into the specifics of dental insurance coverage for root tip removal, we uncover the types of plans that typically provide coverage, examining their provisions and limitations. We also shed light on the factors that insurance companies consider when determining coverage, including the severity of the condition, the complexity of the procedure, and the patient’s overall dental health.
Furthermore, we address pre-existing conditions and exclusions that may impact coverage.
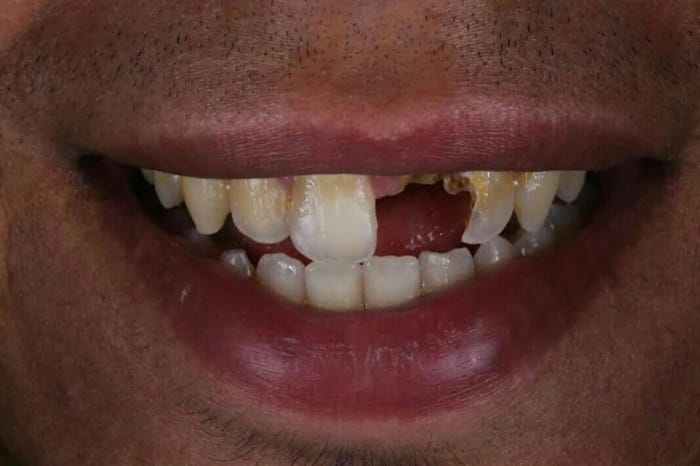
Overview of Root Tip Removal

Root tip removal, also known as apicoectomy, is a dental procedure that involves the surgical removal of the tip of a tooth’s root. This procedure is often necessary when the root tip is infected, decayed, or damaged due to trauma.
By removing the affected root tip, the dentist can eliminate the source of infection or pain and preserve the rest of the tooth.
Causes of Root Tip Removal
There are several common causes that may necessitate root tip removal:
- Infection: When a tooth becomes infected, the infection can spread to the root tip, causing pain, swelling, and bone loss. In such cases, root tip removal may be necessary to eliminate the infection and prevent further damage to the tooth and surrounding tissues.
- Decay: If tooth decay reaches the root tip, it can cause significant damage to the tooth’s structure. Root tip removal may be necessary to remove the decayed portion of the root and prevent further spread of the decay.
- Trauma: Dental trauma, such as a blow to the mouth, can cause the root tip to become fractured or damaged. In these cases, root tip removal may be necessary to prevent further complications, such as infection or pain.
Process of Root Tip Removal
The process of root tip removal typically involves the following steps:
- Local Anesthesia: The dentist will administer local anesthesia to numb the area around the affected tooth.
- Incision: A small incision is made in the gum tissue to expose the root tip.
- Removal of Bone: If necessary, the dentist will remove a small amount of bone to access the root tip.
- Root Tip Removal: Using specialized instruments, the dentist will carefully remove the infected, decayed, or damaged portion of the root tip.
- Filling and Sealing: The remaining root canal is cleaned, shaped, and filled with a biocompatible material to seal the root canal and prevent future infection.
- Suture: The incision in the gum tissue is sutured to close the wound and promote healing.
After the procedure, the patient may experience some discomfort or swelling, which can be managed with over-the-counter pain relievers. It is important to follow the dentist’s instructions for post-operative care to ensure proper healing and prevent complications.
Insurance Coverage for Root Tip Removal

Dental insurance coverage for root tip removal can vary among insurance plans and providers. In general, most dental insurance plans offer some level of coverage for root tip removal, but the specific provisions and limitations may differ.
To determine your coverage for root tip removal, it’s essential to review your dental insurance policy or contact your insurance provider directly. Some common types of dental insurance plans that may cover root tip removal include:
Dental Indemnity Plans
Dental indemnity plans provide coverage for a wide range of dental procedures, including root tip removal. These plans typically offer a fixed reimbursement amount for covered procedures, up to a certain annual maximum.
Dental PPO Plans
Dental PPO (Preferred Provider Organization) plans offer coverage for a network of dentists who have agreed to provide services at a discounted rate. Root tip removal may be covered under a dental PPO plan, but the coverage may vary depending on the specific plan and the dentist you choose.
Dental HMO Plans
Dental HMO (Health Maintenance Organization) plans typically offer comprehensive coverage for a set of covered services, including root tip removal. However, these plans may require you to choose a dentist from a specific network, and coverage may be limited to certain procedures.
In addition to these general types of dental insurance plans, there may be other specialized plans or riders that offer coverage for root tip removal. It’s essential to carefully review your dental insurance policy or contact your insurance provider to determine the specific coverage available for this procedure.
Some examples of dental insurance companies that may offer coverage for root tip removal include:
- Delta Dental
- Cigna Dental
- Blue Cross Blue Shield Dental
- Guardian Dental
- Humana Dental
Please note that the coverage for root tip removal may vary among different plans and providers within these companies. It’s always recommended to contact your insurance provider or review your policy to confirm the specific coverage available for this procedure.
Factors Influencing Coverage
Insurance companies meticulously evaluate various factors when determining coverage for root tip removal procedures. These factors encompass the severity of the condition, the complexity of the procedure, the patient’s overall dental health, and any pre-existing conditions or exclusions Artikeld in the insurance policy.
The severity of the condition plays a pivotal role in coverage determination. Insurance companies are more likely to approve coverage for root tip removal if the condition is severe and poses a significant threat to the patient’s oral health. Conversely, if the condition is mild or manageable with alternative treatments, coverage may be denied.
Complexity of the Procedure
The complexity of the root tip removal procedure also influences coverage decisions. Simple procedures, such as removing a single root tip in an accessible location, are generally covered by insurance. However, complex procedures, such as removing multiple root tips or those located in difficult-to-reach areas, may require prior authorization from the insurance company and may be subject to additional costs.
Patient’s Overall Dental Health
The patient’s overall dental health is another important consideration for insurance companies. Patients with good oral hygiene and a history of regular dental checkups are more likely to receive coverage for root tip removal. Conversely, patients with poor oral hygiene or a history of dental neglect may face challenges in obtaining coverage.
Pre-existing Conditions and Exclusions
Pre-existing conditions and exclusions specified in the insurance policy can also impact coverage for root tip removal. Some insurance policies may exclude coverage for root tip removal if the condition is a result of a pre-existing condition, such as periodontal disease or a failed root canal.
Additionally, certain policies may have annual or lifetime limits on coverage for dental procedures, which could affect the patient’s ability to obtain coverage for root tip removal.
Pre-Approval and Claim Submission
Obtaining pre-approval from your insurance company before undergoing root tip removal is crucial to ensure coverage. Additionally, understanding the claim submission process will help you navigate the reimbursement procedure effectively.
Let’s delve into the process of pre-approval and claim submission for root tip removal.
Pre-Approval Process
Obtaining pre-approval is essential for confirming your insurance coverage for root tip removal. Here’s a step-by-step guide:
- Contact Your Insurance Company: Reach out to your insurance provider either through their customer service hotline, online portal, or mobile application.
- Provide Necessary Information: Be prepared to furnish details about your dental condition, the recommended root tip removal procedure, and the estimated cost.
- Submit Required Documents: Depending on your insurance plan, you may need to submit additional documents, such as a referral from your dentist or a pre-treatment estimate.
- Await Approval: The insurance company will review your request and notify you of their decision. This process may take several days or even weeks.
Claim Submission Process
Once your root tip removal procedure is complete, you can submit a claim to your insurance company for reimbursement. Here’s a step-by-step guide:
- Gather Documentation: Collect all relevant documentation, including the pre-approval letter (if applicable), receipts for the procedure, and any additional documentation requested by your insurance company.
- Complete Claim Form: Obtain a claim form from your insurance company’s website or through their customer service department. Fill out the form accurately and completely.
- Submit Claim: Submit the completed claim form, along with the supporting documentation, to your insurance company. You can do this online, by mail, or through their mobile application.
- Track Claim Status: Keep track of the status of your claim by regularly checking your insurance company’s online portal or by contacting their customer service department.
Coverage for Additional Procedures

In addition to the root tip removal itself, there are several other dental procedures that are often associated with it and may be covered by insurance. These additional procedures can include X-rays, anesthesia, and post-operative care.
X-rays are typically taken before and after root tip removal to assess the extent of the infection and to ensure that the procedure was successful. Anesthesia is used to numb the area around the tooth being treated, making the procedure more comfortable for the patient.
Post-operative care may include pain medication, antibiotics, and follow-up appointments to monitor the healing process.
Impact of Patient’s Dental History and Dentist’s Recommendations
The coverage for additional procedures associated with root tip removal can be influenced by the patient’s dental history and the dentist’s recommendations. For example, if the patient has a history of gum disease or other oral health problems, the insurance company may require pre-authorization for the additional procedures.
Additionally, the dentist’s recommendations for the type of anesthesia and post-operative care may also impact the coverage.
Denied Claims and Appeals

Handling denied claims for root tip removal involves understanding the reasons for denial and following the appropriate appeals process.
In cases where a claim is denied, it’s crucial to review the explanation of benefits (EOB) provided by the insurance company. The EOB typically Artikels the reason for denial, which can range from lack of pre-approval to ineligibility for the procedure.
Once the reason for denial is identified, you can take the necessary steps to address it.
Appeals Process
If you believe the claim denial is incorrect, you can initiate the appeals process by submitting a formal appeal to the insurance company. This typically involves providing additional documentation and information to support the claim.
- Gather Documentation: Collect relevant medical records, including the initial diagnosis, treatment plan, and any supporting documentation from the dentist.
- Write an Appeal Letter: Draft a letter explaining why the claim should be approved. Clearly state the reason for the denial and provide evidence to refute it.
- Submit the Appeal: Send the appeal letter along with the supporting documentation to the insurance company’s appeals department.
The insurance company will review the appeal and make a decision. If the appeal is denied, you may have the option to file an external review or take legal action, depending on the circumstances.
Effective Communication
- Be Clear and Concise: Use clear and concise language in your appeal letter. Avoid using technical jargon that may confuse the insurance company.
- Be Polite and Respectful: Maintain a polite and respectful tone throughout the appeals process. This can help build a positive relationship with the insurance company and increase the chances of a favorable outcome.
- Be Persistent: The appeals process can be lengthy and challenging. It’s important to be persistent and follow up with the insurance company regularly to ensure your appeal is being processed.
Out-of-Network Providers
When considering root tip removal, it’s important to understand the coverage options available if you choose an out-of-network provider.
Out-of-network providers are those who have not entered into a contract with your insurance company. As a result, they are not obligated to accept the insurance company’s reimbursement rates.
Reimbursement for Out-of-Network Coverage
When you receive care from an out-of-network provider, you may be responsible for paying the entire cost of the procedure upfront. However, your insurance company may provide reimbursement for a portion of the cost, depending on the terms of your plan.
The amount of reimbursement you receive will vary depending on your insurance plan and the provider’s fees. In some cases, you may receive reimbursement for the full amount of the procedure, while in other cases, you may only receive a percentage of the cost.
Finding Out-of-Network Providers
If you are considering using an out-of-network provider for root tip removal, it’s important to do your research and find a provider who accepts insurance.
You can start by asking your dentist for recommendations. You can also search online or contact your insurance company for a list of providers in your area who accept insurance for root tip removal.
Dental Savings Plans vs. Insurance
Dental savings plans and traditional dental insurance plans differ in their coverage for root tip removal. Dental savings plans, also known as dental discount plans, are not insurance plans and do not provide coverage for dental procedures. Instead, they offer discounted rates on dental services from participating providers.
Traditional dental insurance plans, on the other hand, provide coverage for a range of dental procedures, including root tip removal, up to a certain limit.
Advantages and Disadvantages
Dental savings plans typically have lower monthly premiums than traditional dental insurance plans, making them a more affordable option for some individuals. However, they do not offer the same level of coverage as traditional dental insurance plans and may not cover all the costs associated with root tip removal.
Traditional dental insurance plans provide more comprehensive coverage for dental procedures, including root tip removal, but they typically have higher monthly premiums.
Factors to Consider
When choosing between a dental savings plan and traditional dental insurance, individuals should consider their budget, their dental needs, and the availability of participating providers in their area. Individuals with limited dental needs or those who are on a tight budget may find a dental savings plan to be a more affordable option.
Individuals with more extensive dental needs or those who are concerned about the cost of root tip removal may want to consider a traditional dental insurance plan.
State-Specific Regulations

Dental insurance coverage for root tip removal can vary across different states due to specific regulations and guidelines. It is crucial to understand these state-specific regulations before undergoing the procedure to ensure coverage and avoid unexpected expenses.
State dental boards and insurance departments play a significant role in regulating dental insurance coverage, including root tip removal. These regulations may include coverage limitations, pre-authorization requirements, and reimbursement rates. Understanding these regulations can help individuals make informed decisions about their dental care and insurance coverage.
Examples of States with Unique Regulations
Some states have unique regulations regarding dental insurance coverage for root tip removal. For instance:
- California: In California, dental insurance plans must cover root tip removal if it is deemed medically necessary by a dentist. However, coverage may vary depending on the specific plan and provider.
- New York: In New York, dental insurance plans are required to cover root tip removal if it is considered a covered service under the plan. The plan must also provide clear information about coverage limitations and exclusions.
- Texas: In Texas, dental insurance plans are not required to cover root tip removal. However, some plans may offer coverage for this procedure as an optional benefit.
These examples illustrate the varying regulations across states, highlighting the importance of checking state-specific regulations before undergoing root tip removal.
Patient Advocacy and Resources
Navigating insurance coverage for root tip removal can be complex. Fortunately, there are resources and organizations dedicated to supporting patients in this process.
Patient advocates play a crucial role in assisting patients with insurance-related issues. They can help patients understand their coverage, negotiate with insurance companies, and file appeals if necessary.
Patient Advocacy Organizations
Numerous organizations provide advocacy and support to patients seeking coverage for root tip removal.
- National Association of Dental Plans (NADP): NADP offers resources and information on dental insurance, including coverage for root tip removal.
- American Dental Association (ADA): The ADA provides information on dental insurance and can connect patients with local dentists who accept their insurance.
- National Consumers League (NCL): The NCL advocates for consumer rights, including access to affordable dental care.
Tips for Communicating with Insurance Companies
Effective communication with insurance companies is key to advocating for coverage.
- Be prepared: Gather all relevant medical records and insurance information before contacting your insurance company.
- Be clear and concise: Explain the situation and your request for coverage in a clear and concise manner.
- Be persistent: If your initial request is denied, don’t give up. Follow up with your insurance company and consider filing an appeal.
Patient Advocates
Patient advocates can provide invaluable assistance in navigating insurance-related issues.
- Understanding coverage: Patient advocates can help patients understand their insurance coverage and determine if root tip removal is covered.
- Negotiating with insurance companies: Patient advocates can negotiate with insurance companies on behalf of patients to obtain coverage for root tip removal.
- Filing appeals: If an insurance claim is denied, patient advocates can assist patients in filing an appeal.
Last Recap

Navigating the complexities of dental insurance coverage for root tip removal requires a comprehensive understanding of the factors influencing coverage, pre-approval processes, and strategies for handling denied claims. By delving into the nuances of dental insurance policies, patients can effectively advocate for coverage and ensure access to necessary dental care.
Whether seeking coverage for root tip removal or other dental procedures, patients should remain informed, proactive, and persistent in their pursuit of appropriate coverage.
FAQs
Does dental insurance always cover root tip removal?
Coverage for root tip removal varies among dental insurance plans. Some plans may provide full coverage, while others may have limitations or exclusions. It’s essential to check with your insurance provider to determine your specific coverage.
What factors influence coverage for root tip removal?
Factors that influence coverage include the severity of the condition, the complexity of the procedure, the patient’s overall dental health, pre-existing conditions, and any applicable exclusions in the insurance policy.
How can I obtain pre-approval for root tip removal?
To obtain pre-approval, contact your insurance provider before undergoing the procedure. They will provide instructions on the pre-approval process, which may involve submitting a pre-treatment estimate or obtaining a referral from your dentist.
What should I do if my claim for root tip removal is denied?
In case of a denied claim, contact your insurance provider to understand the reason for denial. You may be able to appeal the decision by submitting additional information or documentation. If the appeal is unsuccessful, you may consider filing a complaint with your state’s insurance department.