In the intricate world of healthcare, prescription insurance plays a crucial role in ensuring accessible and affordable medications for patients. As a pharmacy technician, you stand at the forefront of this process, serving as a vital link between patients, providers, and insurance companies.
This comprehensive guide delves into the intricacies of prescription insurance, empowering you with the knowledge and skills to navigate this complex landscape effectively and efficiently.
With a clear understanding of prescription insurance plans, key terms, and claim submission processes, you’ll be equipped to assist patients in maximizing their coverage, resolving common issues, and staying up-to-date with evolving regulations. By leveraging technology, fostering effective communication, and adhering to ethical considerations, you’ll not only enhance patient care but also contribute to the overall success of your pharmacy.
Understanding Prescription Insurance

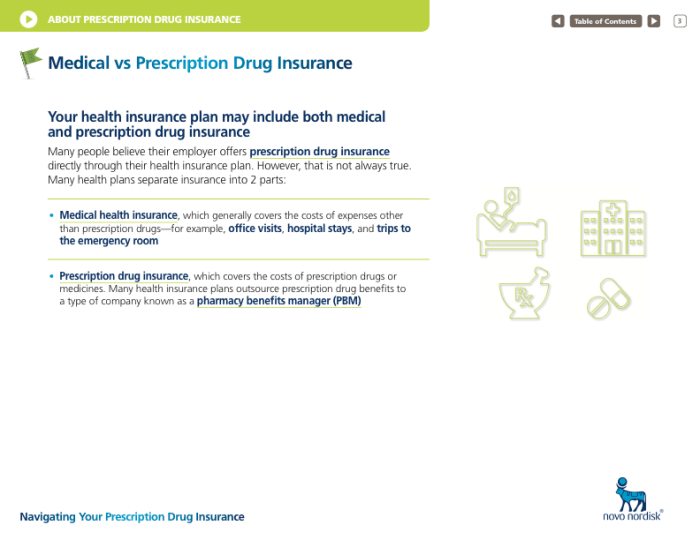
Prescription insurance is a type of health insurance that helps cover the cost of prescription medications. It can be a valuable benefit, especially if you take multiple medications or have a chronic condition that requires ongoing medication.There are different types of prescription insurance plans available, each with its own benefits and limitations.
Some common types of plans include:
- Preferred Provider Organization (PPO): With a PPO plan, you can choose any doctor or pharmacy you want, but you’ll pay less if you use providers within the plan’s network.
- Health Maintenance Organization (HMO): With an HMO plan, you must choose a primary care doctor who will coordinate your care. You can only see specialists if your primary care doctor refers you.
- Point-of-Service (POS): A POS plan is a hybrid of a PPO and an HMO. You can choose any doctor or pharmacy you want, but you’ll pay less if you use providers within the plan’s network.
Prescription insurance plans typically have a deductible, which is the amount you have to pay out-of-pocket before the insurance company starts to cover your costs. Once you meet your deductible, you’ll typically pay a copay, which is a fixed amount you pay for each prescription.
Some plans also have a coinsurance, which is a percentage of the cost of the prescription that you pay.It’s important to understand the key terms and concepts related to prescription insurance so that you can make informed decisions about your coverage.
Here are some common terms to know:
- Copay: A fixed amount you pay for each prescription.
- Deductible: The amount you have to pay out-of-pocket before the insurance company starts to cover your costs.
- Formulary: A list of prescription drugs that are covered by your insurance plan.
- Generic drug: A drug that is the same as a brand-name drug but is sold at a lower cost.
- Preferred drug: A drug that is covered by your insurance plan at a lower cost than other drugs in the same class.
- Prior authorization: A requirement from your insurance company that you get approval before you can fill a prescription for certain medications.
Role of Technicians in Prescription Insurance
Pharmacy technicians play a crucial role in processing prescription insurance claims accurately and efficiently. They are responsible for verifying patient information, insurance coverage, and medication details, ensuring that claims are submitted promptly to avoid delays in reimbursement. Accurate and timely claim submission is essential for patients to receive their medications without financial burden and for pharmacies to receive timely reimbursement for their services.
Assisting Patients in Understanding Prescription Insurance Coverage
Technicians can assist patients in understanding their prescription insurance coverage by providing clear and concise explanations of their benefits, including co-pays, deductibles, and covered medications. They can also help patients identify any potential gaps in coverage and suggest ways to minimize out-of-pocket expenses.
By empowering patients with knowledge about their insurance coverage, technicians contribute to improved medication adherence and overall healthcare outcomes.
Tips for Technicians

Processing prescription insurance claims accurately and efficiently is crucial for technicians to ensure patients receive their medications timely and without financial burdens. Here are some tips for technicians to effectively handle prescription insurance claims:
Understanding Insurance Policies
Technicians should have a thorough understanding of various insurance policies, including coverage details, formularies, and claim submission requirements. Staying updated on policy changes and guidelines is essential to avoid claim denials or delays.
Patient Communication
Communicating clearly and effectively with patients about their prescription insurance coverage is vital. Technicians should explain insurance terms, benefits, and any out-of-pocket costs in a manner that patients can easily understand. Patience and empathy are key to addressing patient concerns and ensuring they receive the necessary support.
Accurate Claim Submission
Accuracy is paramount when submitting prescription insurance claims. Technicians should verify patient information, insurance details, medication dosages, and diagnosis codes to ensure claims are processed correctly. Double-checking all information before submission minimizes errors and delays.
Timely Claim Submission
Promptly submitting prescription insurance claims is essential to avoid claim denials due to late filing. Technicians should be aware of claim submission deadlines and follow up on claims that have not been processed within a reasonable timeframe.
Record Keeping
Maintaining accurate and organized records of prescription insurance claims is crucial for efficient tracking and follow-up. This includes keeping records of claim submissions, payments, and any correspondence with insurance companies. Proper record-keeping facilitates timely resolution of any claim-related issues.
Stay Updated
The healthcare industry is constantly evolving, and staying updated with the latest regulations, policies, and technological advancements is essential for technicians. Attending workshops, seminars, and online courses can help technicians stay current and enhance their skills in processing prescription insurance claims.
Collaboration with Pharmacists
Collaboration between technicians and pharmacists is crucial for effective prescription insurance claim processing. Pharmacists can provide guidance on medication selection, insurance coverage, and any special requirements for specific medications. This collaboration ensures accurate claim submission and timely medication dispensing.
Handling Common Issues
Technicians frequently encounter various challenges while processing prescription insurance claims. Identifying these common issues and developing effective strategies to address them is essential for smooth and efficient claim processing.
To begin with, technicians should be aware of potential claim rejections due to inaccurate or incomplete patient information. This can include incorrect spelling of names, invalid insurance numbers, or missing policy details. Thorough verification of patient data before submitting claims can prevent these rejections.
Troubleshooting Claim Rejections
- Verify Patient Information: Double-check patient details, including name, address, insurance ID, and policy group number, against the insurance card and patient records.
- Review Prescription Details: Ensure that the prescription is valid, has not expired, and includes the correct dosage, quantity, and instructions.
- Check for Prior Authorizations: Certain medications may require prior authorization from the insurance company. Verify if authorization has been obtained before submitting the claim.
- Investigate Formulary Issues: Some insurance plans have formularies that restrict coverage to specific medications. Check if the prescribed drug is included in the patient’s formulary.
- Contact the Insurance Provider: If the claim rejection reason is unclear, contact the insurance company’s customer service department for clarification and guidance.
In addition to claim rejections, technicians may encounter issues related to insurance coverage verification. Patients may have multiple insurance policies, and determining the primary and secondary coverage can be challenging. It is crucial to obtain accurate insurance information from patients and verify their coverage details with the respective insurance providers.
Maintaining Open Communication
Open communication with patients and insurance providers is vital for resolving issues and ensuring timely claim processing. Technicians should clearly explain the claim process and any potential issues to patients. They should also keep patients informed about the status of their claims and any necessary actions required from their end.
Effective communication with insurance providers is equally important. Technicians should be able to articulate the patient’s situation and the rationale behind the prescription. They should also be prepared to provide additional information or documentation if requested by the insurance company.
Staying Up-to-Date

Staying informed about prescription insurance regulations and policies is essential for technicians to provide accurate and efficient customer service. Changes in these regulations can impact patients’ eligibility for coverage, the types of medications covered, and the cost of prescriptions.
Technicians must stay up-to-date on these changes to ensure they are providing the most accurate and current information to patients.
- Regularly review insurance updates and bulletins: Many insurance companies and pharmacy chains provide regular updates on changes to their prescription insurance policies. Subscribing to these updates will keep technicians informed of any new or revised regulations.
- Attend continuing education programs: Continuing education programs are a great way for technicians to stay up-to-date on the latest changes in prescription insurance regulations and policies. These programs can be offered through online courses, webinars, or in-person seminars.
- Network with other technicians: Networking with other technicians is a great way to stay informed about the latest changes in prescription insurance. By sharing information and experiences, technicians can stay up-to-date on the latest developments in the field.
Patient Education
Educating patients about their prescription insurance coverage is a crucial aspect of a technician’s role. Effective patient education ensures that patients understand their benefits, copays, and deductibles, empowering them to make informed decisions regarding their prescription drug therapy.
Technicians can play a vital role in patient education by employing the following strategies:
Clear and Concise Communication
Use clear and simple language to explain insurance coverage details. Avoid technical jargon and acronyms that may confuse patients. Break down complex concepts into manageable chunks of information.
Personalized Approach
Tailor the education to each patient’s individual needs and circumstances. Consider their health literacy, language preferences, and specific concerns. Provide customized guidance that addresses their unique situation.
Utilize Visual Aids
Incorporate visual aids such as charts, graphs, or infographics to illustrate key points and simplify complex information. Visuals can make the information more accessible and engaging for patients.
Provide Written Materials
Offer written materials, such as brochures or handouts, that patients can refer to later. These materials should reinforce the information provided during the verbal education session and serve as a resource for future reference.
Encourage Questions and Feedback
Encourage patients to ask questions and provide feedback throughout the education process. Address their concerns and clarify any misunderstandings. Feedback from patients helps technicians refine their educational approach and improve the overall patient experience.
Collaborate with Other Healthcare Professionals
Collaborate with other healthcare professionals, such as pharmacists or nurses, to provide comprehensive patient education. A team approach can ensure that patients receive consistent and accurate information from multiple sources.
Stay Up-to-Date on Insurance Policies
Stay updated on changes in insurance policies and regulations to provide patients with the most current information. This includes being aware of any changes in formularies, copay structures, or deductibles.
Utilizing Technology
Technology plays a crucial role in enhancing efficiency and accuracy in prescription insurance processing. It streamlines various aspects of the process, enabling technicians to better serve patients and healthcare providers.
Automating Claim Submission
- Electronic claim submission: Utilizing electronic systems to transmit claims directly to insurance companies speeds up the processing time, reducing manual paperwork and minimizing errors associated with manual data entry.
- Real-time claim status tracking: Technology allows technicians to track the status of claims in real-time, providing instant updates on the claim’s progress and any issues that may arise.
Enhancing Patient Experience
- Online portals: Establishing online portals for patients allows them to access their prescription insurance information, view claims history, and make payments conveniently.
- Mobile applications: Developing mobile applications empowers patients to manage their prescription insurance on the go, providing easy access to information and enabling them to communicate with their healthcare providers.
Improving Communication and Collaboration
- Electronic prescribing (e-prescribing): E-prescribing systems enable healthcare providers to send prescriptions electronically to pharmacies, eliminating the need for handwritten prescriptions and reducing the risk of errors.
- Secure messaging: Secure messaging platforms facilitate communication between healthcare providers, pharmacies, and insurance companies, enabling efficient exchange of information and resolution of queries.
Communication and Teamwork

Effective communication and teamwork among technicians, pharmacists, and other healthcare professionals are essential for accurate and timely prescription insurance processing. A collaborative and supportive work environment fosters open communication, shared responsibilities, and mutual respect, leading to improved patient care.
Fostering a Collaborative Work Environment
- Establish Clear Roles and Responsibilities: Clearly define the roles and responsibilities of each team member to avoid confusion and ensure accountability.
- Open Communication: Encourage open and respectful communication among team members, fostering a culture where questions, concerns, and suggestions are welcomed and addressed promptly.
- Regular Team Meetings: Hold regular team meetings to discuss ongoing projects, share updates, address challenges, and celebrate successes, strengthening team cohesion and fostering a sense of共同責任.
- Cross-Training: Promote cross-training opportunities to enhance team members’ skills and knowledge, creating a more versatile and adaptable workforce.
- Peer Support: Encourage peer support and mentorship within the team, fostering a sense of camaraderie and providing opportunities for professional growth and development.
Ethical Considerations
As technicians processing prescription insurance claims, ethical considerations play a crucial role in ensuring patient privacy, confidentiality, and maintaining professional integrity.
Technicians should be aware of the ethical dilemmas that may arise and possess the knowledge and skills to handle them appropriately.
Patient Privacy and Confidentiality
Patient privacy and confidentiality are paramount in healthcare. Technicians must adhere to strict regulations and guidelines to protect patient information.
- Maintain Confidentiality: Technicians must safeguard patient information, including medical history, diagnosis, and treatment details. This information should not be shared with unauthorized individuals or entities.
- Secure Data Storage: Patient data should be stored securely, both physically and electronically. Access to patient records should be restricted to authorized personnel only.
- Patient Consent: In certain circumstances, obtaining patient consent may be necessary before sharing their information. Technicians should clearly explain the purpose of the information sharing and obtain written consent when required.
Conflicts of Interest
Conflicts of interest can arise when personal or financial interests influence professional judgment. Technicians must be vigilant in avoiding situations that may compromise their objectivity.
- Declare Conflicts: If a potential conflict of interest is identified, technicians should promptly disclose it to their supervisor or manager.
- Avoid Financial Incentives: Technicians should not accept gifts, favors, or other inducements from pharmaceutical companies or other entities that may influence their decisions.
- Maintain Professionalism: Technicians should maintain a professional demeanor and avoid engaging in personal relationships with patients or their families that may lead to conflicts of interest.
Integrity and Professionalism
Integrity and professionalism are essential qualities for technicians in the healthcare industry. Maintaining these qualities builds trust and confidence among patients, healthcare providers, and insurance companies.
- Honesty and Transparency: Technicians should always be honest and transparent in their interactions with patients, providers, and insurance companies. Misrepresentation or withholding information can erode trust and lead to ethical violations.
- Accuracy and Attention to Detail: Technicians should strive for accuracy and pay close attention to detail when processing claims. Errors can result in incorrect payments, delays in reimbursement, and patient dissatisfaction.
- Continuous Learning: Technicians should stay up-to-date on changes in insurance regulations, policies, and procedures. Continuous learning ensures that they remain competent and provide accurate and timely services.
10. Continuous Improvement

In the rapidly evolving field of prescription insurance, continuous improvement is not a luxury but a necessity. Technicians must stay abreast of the latest developments, regulations, and best practices to ensure efficient and accurate processing of prescription claims. By identifying areas for improvement, implementing effective changes, and embracing a culture of continuous learning, technicians can significantly enhance the patient experience, optimize operational efficiency, and contribute to the overall success of the prescription insurance ecosystem.
Tips for Identifying Areas for Improvement and Implementing Effective Changes
- Regular Feedback Gathering:
- Continually seek feedback from patients, providers, and internal stakeholders to identify pain points and areas where processes can be streamlined or optimized.
- Data Analytics and Reporting:
- Utilize data analytics tools to analyze claim processing patterns, identify trends, and pinpoint areas with high error rates or inefficiencies.
- Peer Reviews and Collaboration:
- Engage in peer reviews, discussions, and knowledge-sharing sessions with colleagues to exchange ideas and identify potential improvements in existing workflows.
- Industry Trends and Benchmarks:
- Stay informed about industry trends, regulatory changes, and emerging technologies that can potentially revolutionize prescription insurance processing.
By implementing these tips, technicians can proactively identify areas for improvement, develop and test potential solutions, and ultimately drive positive change within the prescription insurance system.
How Continuous Improvement Leads to Better Patient Care and satisfaction
- Enhanced Accuracy and Efficiency:
- By identifying and addressing inefficiencies, technicians can significantly improve the accuracy and efficiency of prescription processing, reducing errors and delays that can cause frustration for patients and providers.
- Optimized Claim Resolution:
- By implementing proactive measures and streamlining processes, technicians can resolve claim issues swiftly, ensuring timely reimbursements for providers and reducing the financial burden on patients.
- Streamlined Communication:
- By utilizing technology and establishing clear communication channels, technicians can facilitate seamless communication with patients, providers, and internal stakeholders, fostering transparency and trust.
- Patient-Centered Approach:
- By continuously seeking ways to improve patient experience, technicians can ensure that the prescription insurance system is patient-centric, addressing their needs and concerns effectively.
Through continuous improvement, technicians can contribute to a prescription insurance system that is more efficient, patient-centered, and responsive to the evolving needs of all stakeholders.
Outcome Summary
As a pharmacy technician, your role in prescription insurance processing extends beyond technical proficiency. You are a patient advocate, a problem solver, and a trusted source of information. By embracing continuous improvement, staying informed about industry changes, and maintaining a patient-centric approach, you’ll not only excel in your profession but also make a meaningful difference in the lives of those you serve.
FAQ Summary
What are the common issues technicians encounter when processing prescription insurance claims?
Incorrect patient information, missing or incomplete documentation, formulary changes, and prior authorization requirements are among the frequently encountered issues.
How can technicians effectively communicate with patients about their prescription insurance coverage?
Clear and concise explanations, active listening, empathy, and patience are key to effective communication with patients regarding their insurance coverage.
What are some best practices for staying up-to-date on changes in prescription insurance regulations and policies?
Regularly reviewing insurance company bulletins, attending industry conferences and webinars, and subscribing to professional journals and newsletters are effective ways to stay informed.
How can technicians utilize technology to improve prescription insurance processing efficiency and accuracy?
Electronic claim submission, e-prescribing, and utilizing software that automates claim processing and eligibility verification can significantly enhance efficiency and accuracy.
What ethical considerations should technicians be aware of when processing prescription insurance claims?
Maintaining patient privacy, avoiding conflicts of interest, and ensuring accurate and timely claim submission are paramount ethical considerations for technicians.